- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2024. 14; 4. DOI 10.35630/2024/14/4.413
Aim: Metabolic syndrome is a complex metabolic disorder that includes a group of co-occurring risk factors, such as obesity, hypertension, hyperglycemia, and hyperlipidemia.
This condition significantly increases the risk of developing cardiovascular diseases and type 2 diabetes, making it a significant public health concern worldwide. Additionally, studies indicate possible links between metabolic syndrome and other conditions, such as dry eye syndrome, suggesting that its impact on health is even broader than previously thought.
The role of metabolic syndrome in the development of dry eye symptoms is still under investigation.This review presents the possible associations between the individual components of metabolic syndrome and dry eye syndrome.
Methods: The research methodology involved conducting a thorough review of scientific articles available through databases such as PubMed and Google Scholar. The team reviewed content from the years 1983–2024, with particular emphasis on the latest advancements. Through systematic organization and validation of the content, 36 of the most reliable publications were highlighted as the basis of the study.
Results: According to the most reliable sources, there is an association between the components of metabolic syndrome and the risk of developing dry eye syndrome.
Conclusions: Based on the literature review, it can be concluded that dry eye syndrome is associated with risk factors of metabolic syndrome, such as hyperglycemia, hypertension, hyperlipidemia, and obesity. The review highlights the need for a holistic approach to patients with dry eye syndrome, including the management of metabolic syndrome risk factors. Effective management of hyperglycemia, hypertension, hyperlipidemia, and obesity may contribute to the reduction of dry eye syndrome symptoms and improve patients' quality of life. Further research is needed to better understand the mechanisms linking these conditions and to develop more effective therapeutic strategies.
Keywords: dry eye syndrome, metabolic syndrome, obesity, hypertension, hyperglycemia, hyperlipidemia
The risk factors for metabolic syndrome encompass four distinct conditions: obesity, hypertension, hyperglycemia, and hyperlipidemia.[26]
The pathophysiology of metabolic syndrome appears to be primarily linked to insulin resistance, with an excessive flow of fatty acids playing a role. Additionally, a proinflammatory state is likely a contributing factor to the syndrome. The elevated risk for type 2 diabetes and cardiovascular disease necessitates targeted therapeutic interventions for individuals at high risk. While the primary strategy involves weight loss and increased physical activity, pharmacological treatment may be warranted for reducing the risk of diabetes and cardiovascular diseases. [9]
Due to the exponential increase in obesity rates, the incidence of metabolic syndrome has risen significantly over the past two decades. [24]
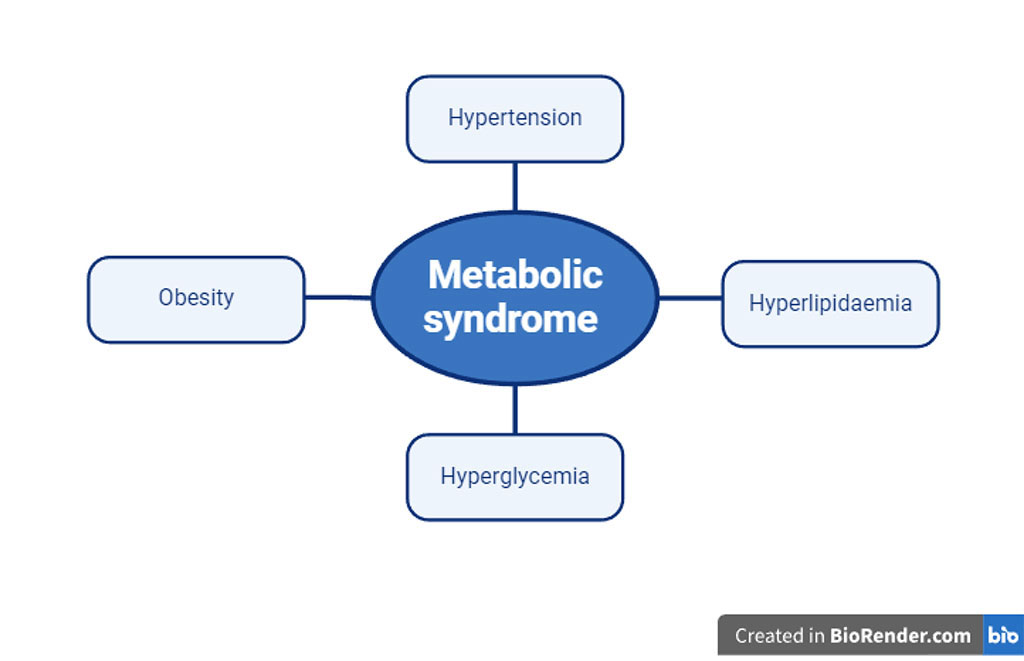
Fig.1. Metabolic syndrome risk factors
Another syndrome that poses a global challenge and is a significant issue affecting many people's lives is dry eye syndrome (DES).
Dry eye syndrome is a complicated multifactorial condition marked by disruptions in the balance of the eye's surface and tear film.[33] It is a condition characterized by redness, burning, a sensation of foreign body and itching. The cause of these symptoms is disturbances in the tear secretion process, their composition, ongoing inflammation, and interference with the integrity of the eye surface structures. [13] Dry eye syndrome may lead to complications such as epithelial deficiency, bacterial keratitis, its melting, and perforation, which are serious ophthalmic conditions.[5]. Dry eye syndrome is among the most common eye conditions, impacting millions of people around the world. Its prevalence varies globally, ranging from 5% to 50% depending on the region.[27] The process of tearing begins in the lacrimal gland located in the upper lateral part of the orbit. Tears bathe the eye and are directed towards the medial portion, where they enter the upper and lower lacrimal puncta. Through the lacrimal canaliculi, tears are transported to the lacrimal sac, from where they reach the nasal cavity via the nasolacrimal duct. [31]
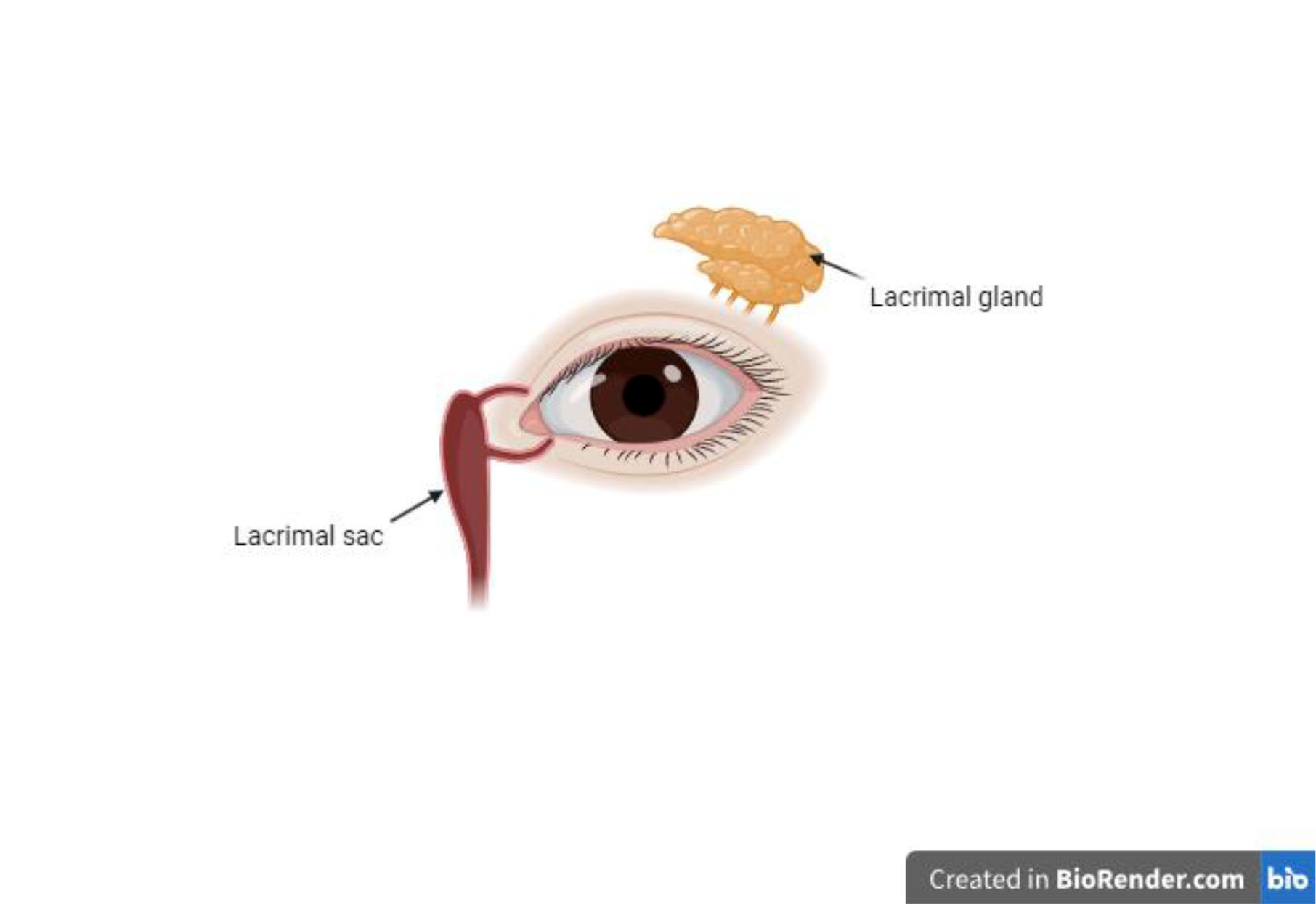
Fig. 2. The lacrimal apparatus
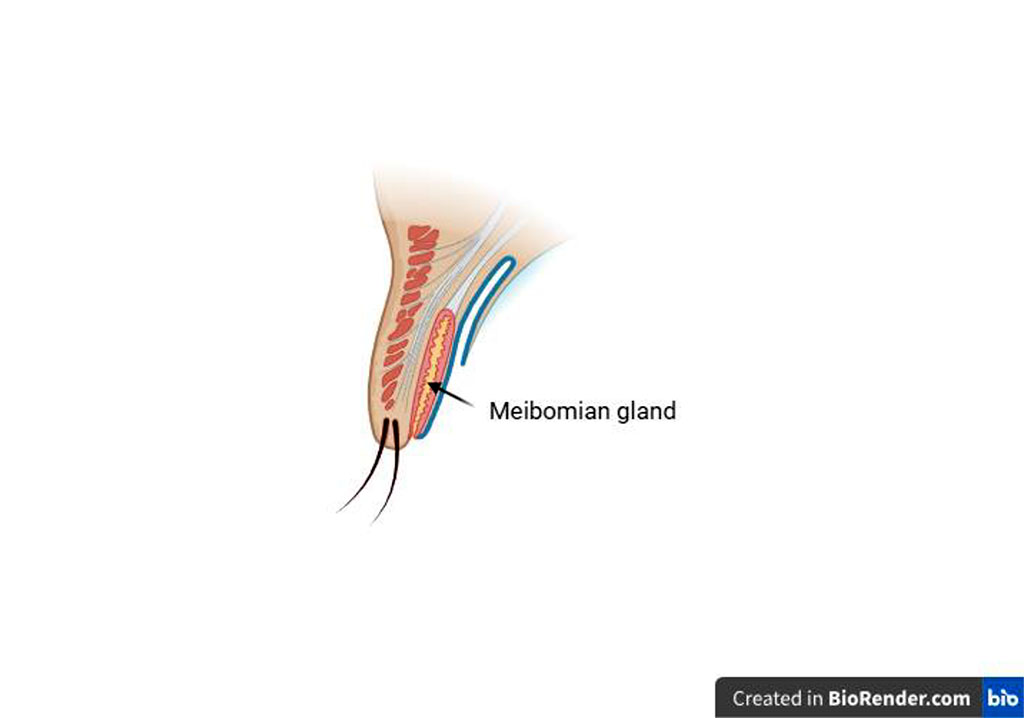
Fig 3. Eyelid anatomy
The tear film consists of three layers: the lipid layer, secreted by the Meibomian glands which are a type of sebaceous glands that are located in the eyelids; the mucin (mucous) layer, mostly secreted by the goblet cells of the conjunctiva, and the aqueous layer, formed by the secretion of the lacrimal glands. Dry eye syndrome occurs when there is a disturbance in the quantity of tears produced, a disturbance in their composition, and there are disorders in the distribution of the tear film - blinking abnormalities .[18]
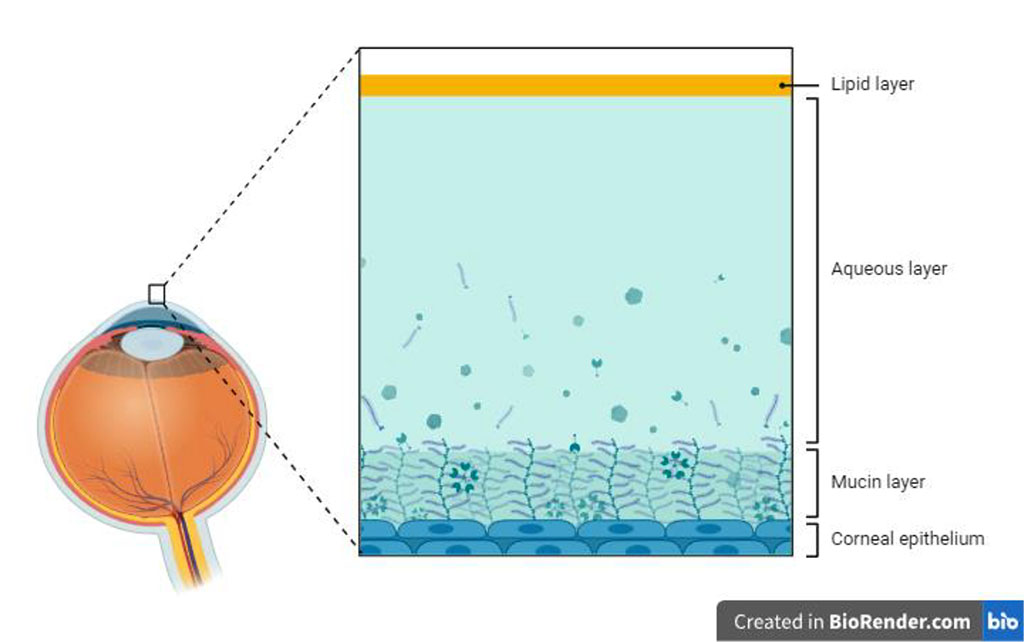
Fig.4 Tear film structure
The core mechanism of dry eye syndrome, according to recent consensus, is the instability of the tear film, and the concept to clarify the cause by focusing on each layer of tear film is referred to as the tear film oriented diagnosis (TFOD). [35]
To check the quantity of the aqueous layer, the Schirmer I test is performed, which comes in two variants: with anesthesia and without anesthesia. The test involves assessing both basal and reflex tearing by inserting a 5 x 35mm strip of filter paper into the conjunctival sac at a distance of 1 ⁄ 3 the length of the eyelid from the outer corner of the eye. A 5 mm segment of the strip remains under the lower eyelid. After 5 minutes, the strip is removed and the result is interpreted. Wetting of more than 15mm of the strip is interpreted as a normal result. The Schirmer I test without anesthesia is at risk of yielding incorrect results because it combines basal secretion with reflex secretion in response to irritation of the conjunctival sac. For a more accurate assessment of basal secretion, the test should be performed with anesthesia. Additionally, the Schirmer I test is prone to error due to the difficulty in maintaining repeatability during the procedure. [6]
To assess the thickness of the lipid layer, interferometry is performed. It allows for the diagnosis of patients with a too thin lipid layer, leading to faster evaporation of the aqueous layer of the tear film.
Assessing the mucin layer currently poses the greatest diagnostic challenge because there are no readily available tests allowing for its evaluation.[32]
To diagnose dry eye syndrome, the tear film break-up time test is also performed. This test involves instilling sodium fluorescein into the patient's eye. The patient is then asked to blink to evenly distribute the fluorescein over the surface of the eye. Examination of the eye is conducted using a slit lamp with cobalt blue light, causing the fluorescein distributed over the surface of the eye to appear green. The time is measured from the blink until the observation of a black spot on the surface of the eye, representing the break-up of the tear film. During diagnosis, it is recommended to perform multiple tests and calculate the average of the results to ensure greater measurement accuracy.
Tear film breakup time (TBUT) is the interval between the blink and the appearance of the first randomly distributed dry spot. A TBUT of less than 10 seconds is considered abnormal.[8]
The foundation of treating dry eye syndrome is diagnosing which component of the tear film is causing it. If disrupted lipid production due to Meibomian gland dysfunction is the cause, treatment involves eyelid hygiene, warm compresses. [17]
Treatment of aqueous layer disorders of the tear film is based on using artificial tear preparations, particularly those containing sodium hyaluronate, and the application of punctal plugs to prevent tear drainage through the natural pathway. [34]
In this study, we aim to analyze the relationship between dry eye syndrome and metabolic abnormalities that are part of the metabolic syndrome.
Measuring fasting glucose levels is a simple and very common test worldwide and serves as the basis for diagnosing diabetes, which is one of the major challenges of modern medicine.
A study by K. Ogurtsova et al. forecasts that by 2040, the rate of diabetes among adults is expected to reach 10.4%.[21]
In a study conducted by Gagandeep K. Brar et al., it was shown that there is an association between fasting blood glucose levels and dry eye syndrome.Of the 200 patients in this study, 63 were diagnosed with dry eye disease, and their average fasting blood sugar was 156.37. In contrast, the 137 patients without dry eye disease had an average FBS of 125.47. [4]
A parameter closely related to blood glucose levels is the level of glycosylated hemoglobin. The hemoglobin A1c (HbA1c, also known as glycated hemoglobin or glycosylated hemoglobin) test assesses how well a person's blood glucose has been controlled. It provides an average of blood sugar levels over the previous 90 days and is expressed as a percentage. [11] The documented prevalence of dry eye syndrome among diabetics ranges from 15% to 33% in individuals aged 65 and older, with the incidence increasing with age. Additionally, dry eye syndrome is approximately 50% more common in women than in men. [36] In a study conducted in a hospital setting, 54% of individuals with diabetes were found to have dry eye syndrome, and there was a notable correlation between the presence of dry eye syndrome and the duration of diabetes. [19]
The result of this study is contrary to the findings of the study conducted by Gagandeep K. Brar et al., which showed that a significant association was found between the duration of diabetes and the presence of dry eye.[4]
In a study conducted by Thang Tran Tat et al. development of dry eye in type 2 diabetes is primarily associated with peripheral corneal neuropathy, instability of the tear film, inflammation of the ocular surface, and apoptosis of conjunctival epithelial cells. [30]
Systemic arterial hypertension is the most significant modifiable risk factor for overall morbidity and mortality globally and is linked to a heightened risk of cardiovascular disease (CVD). [22]
In 2010, approximately 1.38 billion individuals, representing 31.1% of the global adult population, were diagnosed with hypertension, characterized by a systolic blood pressure (BP) of 140 mmHg or higher and/or a diastolic BP of 90 mmHg or higher. [20] The fact that hypertension is a risk factor for many diseases worldwide raises the question of whether it is also a risk factor for dry eye syndrome.
Recent studies have shown that elevated blood pressure is also a risk factor for the development of dry eye syndrome. The mechanism behind this phenomenon involves the presence of a systemic inflammatory state in individuals with hypertension. [34] In a study conducted by Tran Tat Thang et al., 180 out of 432 patients with hypertension met the criteria for dry eye syndrome, accounting for 41.7% of the patients. [29] Moreover, Arthur Ferrero’s et al. study indicated that systemic hypertension was one of the associated factors with dry eye syndrome. [12]
It seems reasonable to ask whether lifestyle changes recommended for people with hypertension, such as physical activity or a Mediterranean diet, also impact the symptoms of dry eye syndrome.[2] Ismail et al. assessed the impact of lifestyle changes as an adjunctive treatment for dry eye syndrome in a randomized, controlled trial involving sixty obese hypertensive adults with DES. They found that obese patients with dry eye who adhered to a physical activity regimen for six months—consisting of thirty minutes of vigorous aerobic exercise three times a week—either alone or combined with a Mediterranean diet, showed significant improvements in dry eye symptoms. These improvements, measured both subjectively and objectively, were more pronounced in the group following the low-calorie Mediterranean diet. [16]
Lipid metabolism disorders are a significant global health issue and a major risk factor for various diseases. The tear film includes a lipid layer produced by the meibomian glands. Therefore, in our study, we aim to investigate whether scientific literature has identified a potential link between hyperlipidemia and dry eye syndrome.
A study by Puneet S. Braich et al. revealed that dyslipidemia, characterized by a fasting total cholesterol level of ≥ 200 mg/dL, triglycerides ≥ 150 mg/dL, LDL ≥ 130 mg/dL, or HDL ≤ 40 mg/dL, was observed in 70 cases (64%) and 21 controls (18%). [4] A study conducted by Banait et al. also noted a relationship between meibomian gland dysfunction and lipid levels. Specifically, the results suggest that meibomian gland dysfunction is positively correlated with elevated levels of LDL, total cholesterol, and triglycerides. [2] In study performed at the University of North Carolina it was shown that dyslipidemia is associated with an increased odds of having a DED diagnosis. [1]
In 2020 study published by Hye Rin Choi et al. suggested that dyslipidemia may be associated with the prevalence of dry eye syndrome in Korean men, but not in women.[7] However, Krishnamoorthy Rathnakumar's et al. study demonstrated that both men and women with dry eye disease (DED) had a statistically significant association with dyslipidemia when compared to those without dry eye.[23]
Obesity is a long-term condition that significantly raises the risk of death and illness, including various cancers, heart disease, disability, diabetes, high blood pressure, osteoarthritis, and stroke. For adults, being overweight is classified as having a body mass index (BMI) between 25 and 29 kg/m², while obesity is defined as a BMI over 30 kg/m². If present trends persist, projections suggest that by 2030, 38% of the global adult population will be overweight, with an additional 20% being obese. [25]
In obesity, the source of low-grade inflammation is adipose tissue, which is abundant in proinflammatory macrophages that generate inflammatory markers. These markers negatively affect tear production, thereby establishing a pathogenic link between obesity and dry eye disease. [28] In the study by Sevil Karaman Erdur et al., it was shown that obesity is a significant risk factor for tear film osmolarity. [10]
In a preliminary, prospective, cross-sectional study by Kam Chun Ho, an association between body fat percentage and dry eye symptoms in the general adult population. [15]
Based on the literature review, it can be concluded that dry eye syndrome (DES) is associated with risk factors that are part of metabolic syndrome, such as diabetes, hypertension, hyperlipidemia, and obesity. Each of these factors plays a significant role in the pathogenesis of DES, affecting various aspects of ocular physiology and tear production mechanisms.
The findings of the review highlight the need for a holistic approach in treating patients with dry eye syndrome. It is crucial not only to address the direct symptoms of DES but also to effectively manage the metabolic syndrome risk factors that may worsen eye health. Managing comorbid conditions such as diabetes, hypertension, hyperlipidemia, and obesity is fundamental in reducing DES symptoms and improving patients' quality of life.
Further research is necessary to better understand the complex mechanisms linking these health conditions and to develop more effective and targeted therapeutic strategies. Such studies should focus on uncovering new pathophysiological pathways, identifying predictive biomarkers, and developing innovative treatment methods that can be applied in clinical practice, offering tangible benefits to patients.