- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 3. DOI 10.35630/2025/15/3.318
Aims: Purpose of this case report is to increase awareness of a rare zoledronic acid side effect which is acute anterior uveitis. We would like to educate both clinicians and patients about possible ocular symptoms that can occur after zoledronic acid administration. As an effect when patients develop these symptoms, they can get optimal medical care as soon as possible and minimize the risk of severe ocular complications.
Case Description: We report a case of an unilateral acute anterior uveitis in a 69 years old woman with osteoporosis secondary to breast cancer treatment who presented with flu-like symptoms accompanied by visual symptoms such as redness, pain and foreign body feeling in the right eye after receiving zoledronic acid infusion. Other causes of uveitis were excluded and after proper treatment symptoms reduced.
Outcomes: The inflammation resolved within two weeks of treatment, with no recurrence or long-term complications during follow-up. Posterior synechiae were successfully released, and visual acuity returned to baseline.
Conclusions: Although the risk of acute anterior uveitis after zoledronic acid infusion is low, it is essential that patients receiving this kind of treatment were properly informed about possible ocular side effects and need for ophthalmological visit if any eye symptoms occur to ensure early diagnosis and prompt accurate treatment.
Keywords: zoledronic acid, zoledronate, acute anterior uveitis, uveitis, case report, adverse drug reactions
Uveitis is the process of inflammation of the uvea, localised in the iris, ciliary body and/or choroid. The most frequent form of uveitis is the anterior uveitis [1]. The incidence rate of this disease is estimated to be 17 to 52 cases per 100000 persons [2]. Although 48 to 70% of anterior uveitis cases are considered to be idiopathic, among other causes HLA-B27-diseases, juvenile idiopathic arthritis, inflammatory bowel disease, sarcoidosis, Behcet’s disease, tubule-interstitial nephritis, bacterial, viral and parasitic diseases are listed [1]. Medications like antiviral drugs, checkpoint inhibitors, and bisphosphonates can also cause anterior uveitis [1,3].
Zoledronic acid-induced uveitis presents mainly as anterior uveitis and occurs usually within 72 h after the first dosage of zoledronic acid with median time to onset around 48 h [4]. Acute anterior uveitis may affect one or both eyes, the symptoms include pain, blurred vision, photophobia and redness [1,4]. The patient can present himself with constriction or irregularity in the shape of the pupil, symptoms caused by the posterior synechiae (adhesion of the iris to the lens). Using a slit lamp the physician may find ciliary flush - cells in the anterior chamber, which can create hypopyon. Other features visible in the slit lamp examination include flare in the anterior chamber and keratic precipitates [1,5]. The treatment of the anterior uveitis consists primarily of topical corticosteroids and cycloplegics. Corticosteroids e.g. dexamethasone or prednisolone are used because of their anti-inflammatory effect, although one of the possible side effects of this therapy may be increase in intraocular pressure (IOP). Therefore, monitoring the IOP is recommended during the treatment. Cycloplegics such as atropine reduce symptoms of anterior uveitis and prevent development of posterior synechiae. Sometimes use of systemic steroids may be needed [1,4]. Patients who discontinue administration of zoledronic acid and receive symptomatic therapy are not at danger for long-term consequences or loss of vision [5].
Bisphosphonates bind themselves into hydroxyapatite in the bones and impact function of osteoclasts, therefore inhibiting bone resorption process. To this drug group belongs zoledronic acid. It is given intravenously in treatment of osteoporosis, glucocorticoid-induced osteoporosis, malignancy-related hypercalcemia, Paget disease and bone metastases [3,6]. Standard therapy consists of injecting 4 to 5 mg once in 12 months which leads to better compliance and efficacy of therapy especially for patients on long-term anti-osteoporosis therapy [3,5]. Due to low frequency of administration and high potency, zoledronic acid is often prescribed for patients who do not tolerate oral bisphosphonates or have bone metastases [5,7]. Side effects of zoledronic acid consist of flu-like symptoms, fever, muscle/joint pain, nausea, fatigue, hypocalcemia, osteonecrosis of the jaw and ocular adverse effects i.e. uveitis, conjunctivitis and scleritis [3,7,8,9,10]. In Patel’s 2014 double-blind, placebo-controlled trial the prevalence of acute anterior uveitis after single injection of zoledronate was established to be 1.1% [11].
We report a case of unilateral acute anterior uveitis in a 69 year old woman with a medical history of hypothyroidism and breast cancer who presented side effects of zoledronic acid administration. The patient has not undergone any previous ophthalmological treatment, except for corrective eyewear. She was treated with zoledronic acid because of osteoporosis induced by treatment of breast cancer with letrozole. 24 hours after first zoledronic acid infusion, patient presented flu-like symptoms, such as muscle pain, weakness, which she was warned about, and also ocular symptoms: redness of the left eye, pain of the left eyeball during eye movements and a feeling of a foreign body under the eyelid. After 48 hours from zoledronic acid infusion blurry vision has occurred. Patient took 200 mg of ibuprofen per os with no result. 72 hours from infusion flu-like symptoms disappeared, however vision problems were progressing. She went to the ophthalmologist who diagnosed her with anterior uveitis and administered topical dexamethasone 0,1% 1 mg/ml every 1 hour, topical ofloxacin 0.5% 5 mg/ml every 2 hours and topical tropicamide 1% 10 mg/ml every 3 hours.
96 hours after infusion, the patient visited the ophthalmic emergency room, where presented best-corrected visual acuity 0.1 (20/200) in the right eye and 1.0 (20/20) in the left eye. Intraocular pressure 14 mmHg right 11 mmHg left. Right eye: conjunctiva with ciliary injection, cornea exhibiting isolated folds of Descemet's membrane at the centre, with endothelial adhesions and newly forming deposits. The anterior chamber was moderately deep, with a Tyndall effect 1+ according to the SUN Working Group classification. The iris showed posterior circular synechia, with a non-reactive, narrow pupil. The lens was cataractous. Fundus examination revealed a pink reflex. Ultrasound of the vitreous body was clear, with no significant pathologies at the posterior pole.
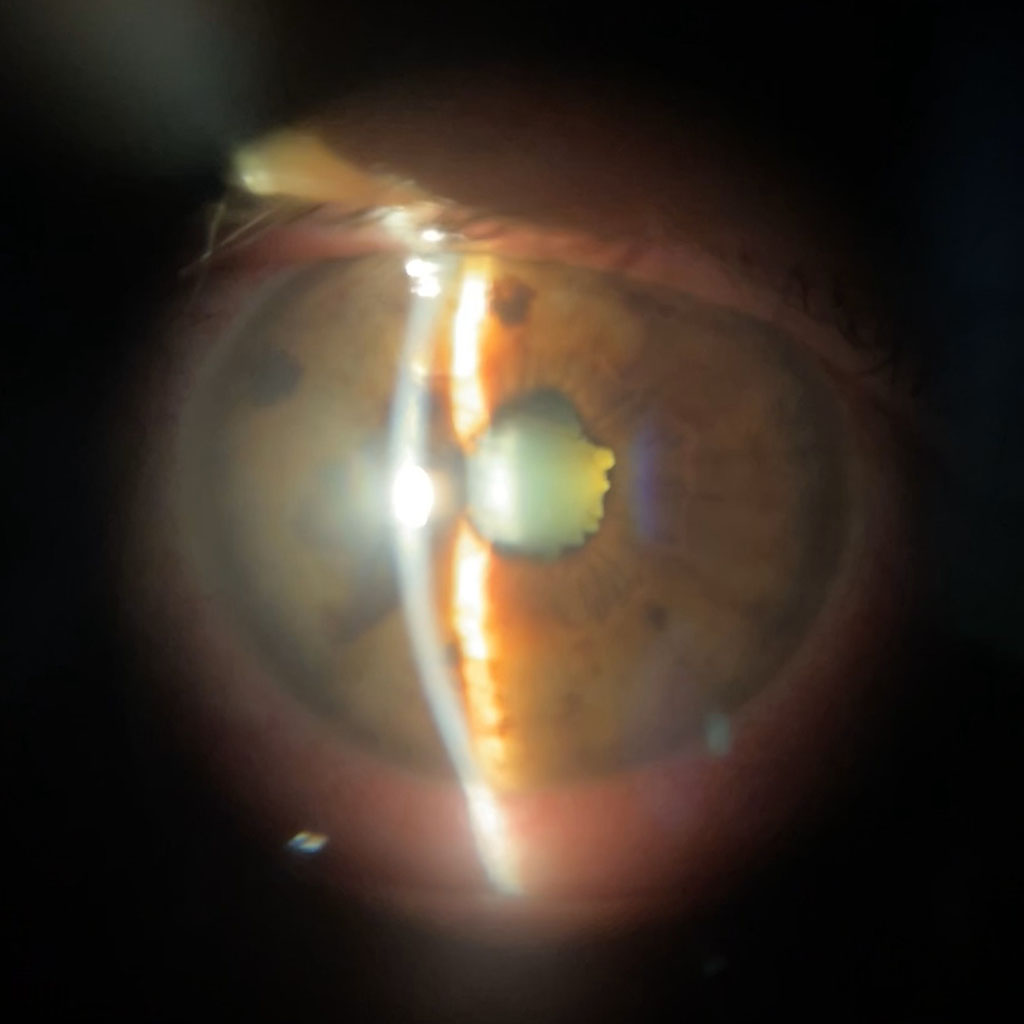
Figure 1. Posterior synechiae in active acute anterior uveitis
The following laboratory tests were performed: complete blood count with differential, ALT, AST, ESR, CRP, serum glucose, electrolyte panel, creatinine, quantitative rheumatoid factor, antinuclear antibodies screening test, Lyme disease IgM and IgG, Toxoplasmosis IgM and IgG, syphilis test, and HLA-B27 antigen.
Imaging tests were also conducted, including X-ray of the sacroiliac joints and paranasal sinuses, as well as a computed tomography scan of the head and orbits, both with and without contrast. A dental consultation was also scheduled.
The following treatment regimen was initiated:
Daily sessions for pupil dilation were performed according to the following schedule 0-10-20-30 minutes:
One hour after the first session for pupil dilation and subconjunctival injection of dexamethasone phosphate, successful disruption of the posterior synechiae was achieved.
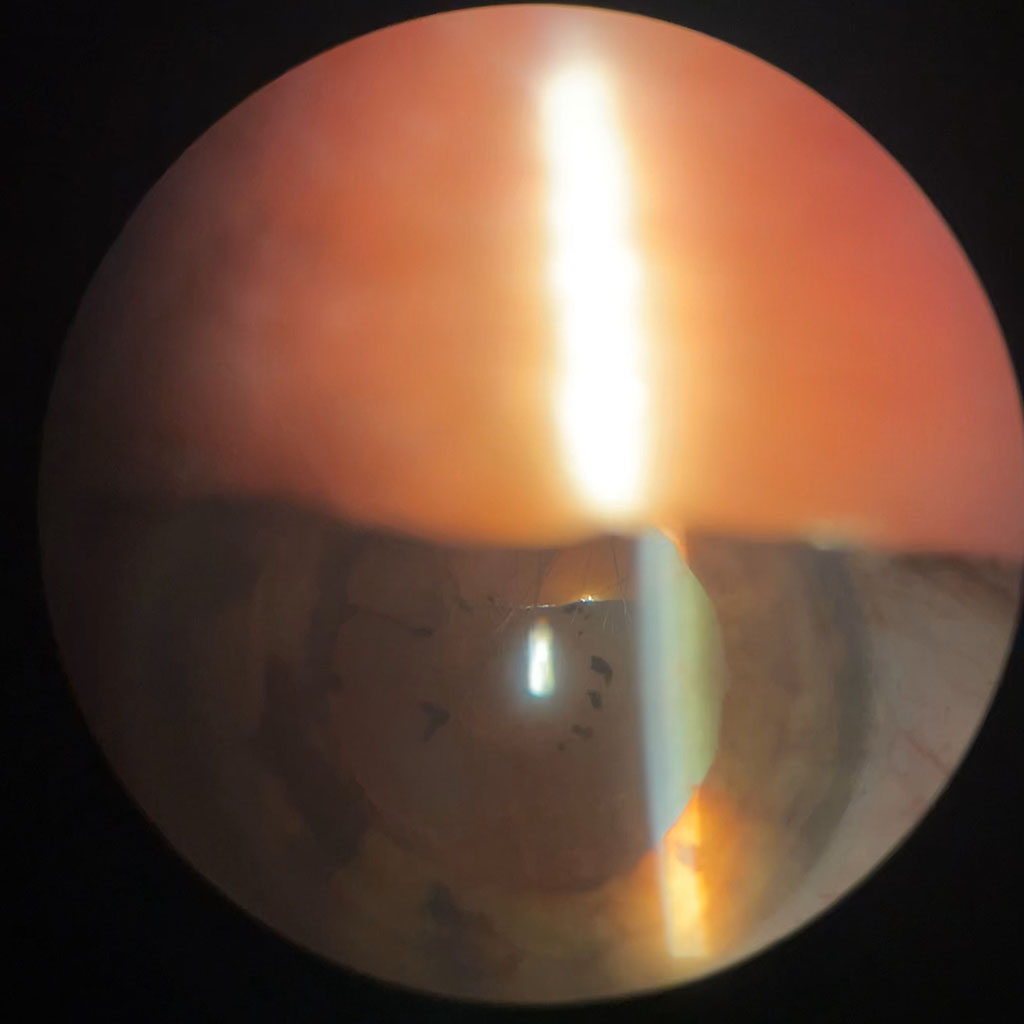
Figure 2. Released posterior synechiae in a patient with acute anterior uveitis
Regarding deviations in laboratory tests: upon admission, CRP was 1.23 mg/dL (reference range: 0.00–0.50), and ESR was 22 mm/h (reference range: 1–20), toxoplasmosis IgG was 2459.000 U/ml, while toxoplasmosis IgM was negative, indicating a previous infection. Other laboratory tests were within normal limits. Imaging studies revealed no identifiable causes for the uveitis. Dental examination showed no signs of inflammatory foci.
Based on the clinical history and obtained test results, the cause of the anterior uveitis was attributed to a zoledronic acid injection.
The patient remained hospitalized for 6 days. On the third day, she reported a burning sensation in the right eye, which resolved after switching treatment from topical dexamethasone to topical loteprednol etabonate 0.5% 5mg/ml 6 times daily. At discharge, the following measurements were recorded: best-corrected visual acuity 0.4 (20/50) in the right eye and 1.0 (20/20) in the left eye, intraocular pressure of both eyes 16 mmHg. The mobility and alignment of the eyeballs were normal, and the pupillary reaction was appropriate. Right eye: the conjunctiva was mildly irritated with deep injection; the cornea was smooth, shiny, and transparent; the anterior chamber was moderately deep and clear; the iris exhibited normal trabecular structure; the pupil was wide, round, and freely reactive; the lens was cloudy with a pigment ring on the anterior capsule from ruptured posterior synechiae. The fundus examination was within normal limits. Laboratory tests showed normalization of inflammatory markers. The patient was prescribed topical loteprednol etabonate 0.5% 5 mg/ml (5 times daily until the follow-up visit) and advised to attend a follow-up appointment at the ophthalmology clinic after 7 days. The inflammation resolved within two weeks of treatment, with no recurrence or long-term complications during follow-up. Posterior synechiae were successfully released, and visual acuity returned to baseline.
The precise mechanism of zoledronic acid induced uveitis remains unclear. However, it is believed that anterior uveitis develops as a result of inflammatory response to zoledronic acid infusion [12]. Administration of nitrogen-containing bisphosphonates such as zoledronic acid may trigger the acute phase reaction (APR) induced by lymphocyte T activation. Non-peptidic antigens like isopentenyl pyrophosphate and dimethylallyl pyrophosphate, which are accumulated due to inhibition of the mevalonate pathway caused by zoledronate, are being recognized by lymphocytes T. Subsequently activated T cells release pro-inflammatory cytokines such as interleukin 6 (IL-6), interleukin 1 (IL-1), tumour necrosis factor alpha (TNF-α) and interferon-gamma (IFN-γ), which may induce a systemic inflammatory response and initiate inflammation in eye structures e.g. uvea, causing as an effect development of acute anterior uveitis. Systemic symptoms of APR following nitrogen-containing bisphosphonates administration include fever, musculoskeletal pain, swelling of joints, nausea, fatigue and others [7,12,13,14]. Time from zoledronic acid infusion to development of acute anterior uveitis symptoms, mostly inflammatory nature of acute anterior uveitis and prompt response to immunosuppressive steroids support the acute phase reaction theory of these condition [12,13]. Regardless of anterior uveitis etiology its complications remain the same and include cataract followed by vision loss, macular oedema and glaucoma [15]. However, when zoledronic acid-induced anterior uveitis is diagnosed early and managed properly patients should not develop severe complications [13].