- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 2. DOI 10.35630/2025/15/2.213
Bullous pemphigoid of pregnancy (pemphigoid gestationis) is a rare autoimmune blistering dermatosis that occurs exclusively during gestation and the postpartum period. The condition is characterized by pruritic erythematous plaques and blistering eruptions, most commonly affecting the abdomen and extremities, while sparing the face and mucous membranes. This disease is associated with significant maternal discomfort and may impact fetal health. Diagnosis is based on a combination of clinical presentation, histopathology, and immunofluorescence findings demonstrating linear deposition of complement C3 and IgG at the dermoepidermal junction.
This article presents a detailed clinical observation of a 37-year-old woman with a history of recurrent bullous pemphigoid associated with three consecutive pregnancies. The diagnosis was confirmed via histological and immunological methods. The patient responded favorably to systemic glucocorticoids and topical therapy, demonstrating resolution of lesions with residual post-inflammatory pigmentation. The case highlights the chronic, relapsing nature of the disease and its tendency to recur in future pregnancies.
The therapeutic approach must balance effective symptom control with safety for both mother and fetus. A multidisciplinary team involving dermatologists, obstetricians, and immunologists is essential for optimal management. This case underlines the importance of early recognition, differential diagnosis, and individualized treatment planning in pregnant patients with autoimmune skin diseases.
Keywords: pregnancy dermatoses, bullous pemphigoid of pregnancy, pemphigoid gestationis, autoimmune disease, diagnosis
There are a number of adaptive processes during pregnancy that affects all organs and systems, including the skin. These changes occur as a result of endocrine and immunological restructuring of the body. There is also an increase in humoral immunity and the production of Th2 cytokines (IL-4, IL-10) in pregnancy. Subsequently, cellular immunity and the production of Th1 cytokines (IL-2, IFN-γ, IL-12) are inhibited under the influence of cytokines, high levels of estrogens, progesterone and chorionic gonadotropin. All these changes lead to physiological immunosuppression, which triggers the onset or exacerbation of various types of dermatological diseases [3,5,8,9].
The complexity of the disease at this stage arises from the limited range of therapeutic options and the possible risk to the fetus. In the group of these diseases, bullous pemphigoid has the most serious prognosis among the disease groups. The evidence of the autoimmune nature of BP is the long-term circulating antibodies to the BP 180 and BP 230 proteins that persist after delivery and complete disappearance of symptoms of dermatosis. BPP is associated with the presence of histocompatibility antigens HLA DR3 and DR4. The primary immune response occurs inside the placenta. Circulating antibodies binding to skin antigens cross-react with the basement membranes of the chorionic epithelium and amnion, and immune complexes are deposited in the placenta. Autoimmune reactions occurring in the skin are associated with the accumulation of immune complexes, activation of complement, chemotaxis, and degranulation of eosinophils, resulting in tissue damage and blistering [4,10,14,16].
Pregnant pemphigoid belongs to the group of so-called dermatoses of pregnancy. This group also includes: polymorphic eruption of pregnancy, intrahepatic cholestasis and atopic dermatitis of pregnancy [1,2,6,7]. Bullous pemphigoid is characterized by recurring with subsequent pregnancies, menstruation, taking oral contraceptives by women suffering from PD (20-50% of cases) [8].
The primary clinical manifestations of bullous pemphigoid in pregnant women are severe itching and erythematous rashes on the skin of the abdomen. The most frequent localization is the umbilical region and extremities. Lesions of the facial skin and oral mucosa are not observed [4,12,14].
Direct immunofluorescence plays a leading role in the diagnosis of BPP. It makes it possible to detect the linear accumulation of complement C3 and IgG autoantibodies in the junction of dermis and epidermis. At the same time, component C3 is detected in all cases of bullous pemphigoid, whereas IgG autoantibodies are detected in 25-50% of cases. Enzyme immunoassay is also used as a diagnostic method, aimed at detecting circulating IgG antibodies to extracellular proteins BP 180 and BP 230. Histological examination of a skin biopsy reveals changes depending on the stage and severity of the process. At the initial stage there is an edema of the upper and middle layers of the dermis, which is accompanied by the formation of a perivascular inflammatory infiltrate consisting of lymphocytes, histiocytes and eosinophils. As it progresses, subepidermal blisters form in the area of the basement membrane [4,10,12,16].
Drug therapy for pregnant women and during breastfeeding requires a special safe approach. Thus, the use of systemic drugs is excluded, if possible. Also topical corticosteroids are recommended to be used in short courses. Topical treatment with emollients and antipruritic agents is preferred, as it includes moisturizing ingredients and tannins that do not adversely affect the course of pregnancy and fetal development. However, in severe cases, it is possible to use the systemic glucocorticoids such as prednisone and methylprednisolone from the 16th week of gestation for rapid and persistent relief of skin condition [8,13,15]. A multidisciplinary approach involving dermatologists, obstetricians, and immunologists is essential for optimizing treatment outcomes while minimizing risks to the fetus.
As an example, the case of bullous pemphigoid in a woman during a third planned pregnancy is presented in the article.
The patient, 37 years old, on 02/27/2024 visited a dermatologist at Avaev Center for Specialized Medical Care (Tver, Russia). She complained of widespread rashes on the skin of the trunk and extremities, accompanied by intense itching.
The general condition was satisfactory, the body temperature was 36.6 C. The examination revealed that the rashes were located on the skin of the trunk, upper and lower extremities. The rash elements were located in the chest, abdomen, lateral surfaces of the chest on the body and mainly in the lumbar region on the back (Fig.1).

Fig 1. Patient P., 37 years old. Erythematous rash on the skin of the trunk
Subsequently, the rashes spread to the flexor surfaces on the extremities (Fig. 2).

Fig. 2. Patient P., 37 years old. Target-like erythematous rashes. Grouped erosions and crusts on the surface of erythema.

Fig.3 Patient P., 37 years old. Blistering rashes on the background of erythema. Multiple excoriations on the skin in the ankle joint and arch of the foot.
The skin outside the lesion was of its usual color and retained its normal appearance and properties. There were no rashes on the mucous membranes of the oral cavity and genitals. The lymph nodes were without features. The general condition of the patient was not disturbed.
In the general blood test: hematocrit 42.8%, hemoglobin 14.2 g/dl, erythrocytes 5.04 ×10⁶/µL, MCV 84.9 fL, RDW 16.7%, MCH 28.1 pg, MCHC 33.2 g/dl, platelets 336 ×10³/µL, leukocytes 10.06 thousand/ml, neutrophils (total 51.3%), lymphocytes 22.6 %, monocytes 4.9%, eosinophils 21%, basophils 0.2 %, neutrophils, abs. 5.17 thousand/ml, lymphocytes, abs. 2.27 thousand/ml, monocytes, abs. 0.49 thousand ml, eosinophils, abs. 2.11 thousand/ml, basophils, abs. 0.02 thousand/ml, ESR 5 mm/h. In the biochemical analysis of blood: ALT 16 U/L, AsAt 15 U/L, Total Bilirubin 9.1 mmol/L, Direct Bilirubin 3.0 mmol/L, Indirect Bilirubin 6.1 mmol/L, Gamma-HT 10 U/L, Glucose 5.2 mmol/L, Creatinine 58 mmol/L, Urea 6.8 µmol/L, Total protein 67 g/L, Alkaline phosphatase 99 U/L, CRP 7.6 mg/L, Ferritin 59 µg/L. The concentration of Ig E is 35 IU/ml.
Microscopic description of the skin punch biopsy: a perivascular infiltrate was detected in the reticular layer of the dermis. It consisted of lymphoid cells with an admixture of a small number of eosinophilic granulocytes. A subepidermal blister with the roof of the entire thickness of the epidermis was located. The cells of the epidermis were stretched; the intercellular bridges of the spiny layer were not affected. There was ballooning degeneration in the spiny layer of the epidermis.
Prediagnosis: the revealed morphological pattern might correspond to pemphigoid gestationis (Fig.4).
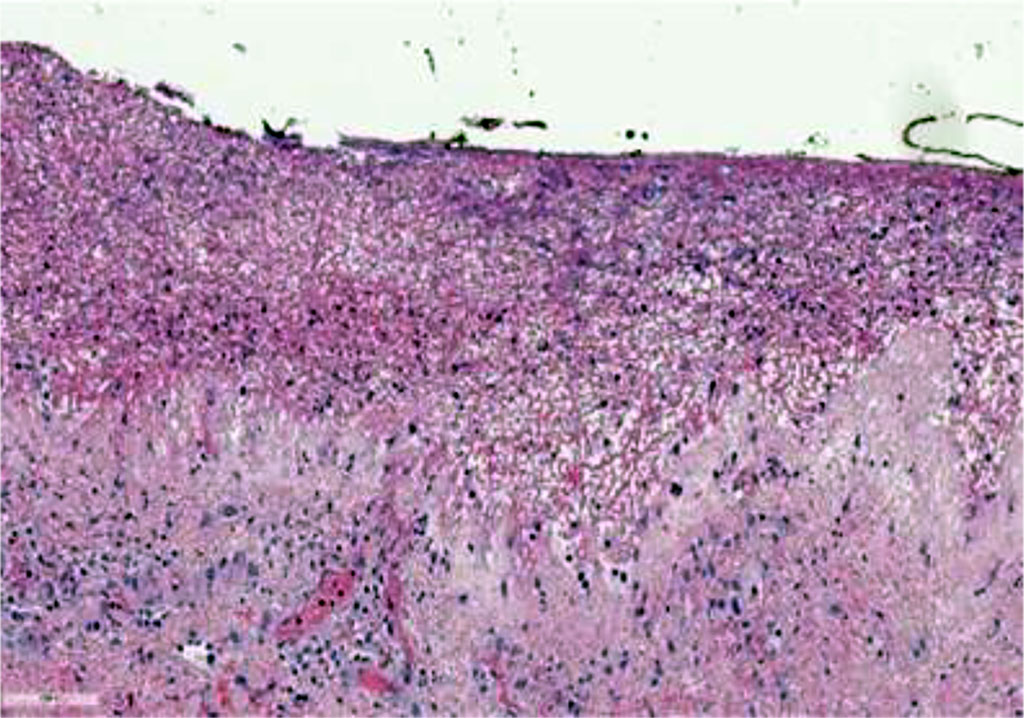
Fig. 4. Histological picture of bullous pemphigoid in pregnancy, hematoxylin and eosin staining (×75)
Based on the patient's complaints, medical history (characteristic chronic course associated with pregnancy), clinical picture and morphological examination data, the diagnosis was established: Pemphigoid of pregnancy (ICD-X: O26.4- Herpes of pregnancy).
Treatment was performed: methylprednisolone 24 mg per day orally in two doses. Рotassium preparations, proton pump blockers, external aniline dye (methylene blue 1% aqueous solution) for erosion and crusts; mometosone furoate 0.1% ointment for edematous erythema.
This clinical case is of interest as a rare autoimmune dermatosis associated exclusively with pregnancy. Skin lesions of a pregnant woman in the postpartum period can be widespread with diverse clinical manifestations and itching can be intense. Rashes often clear in the postpartum period on their own, in other cases, the prescription of systemic glucocorticoids is required. In the absence of future pregnancies, the prognosis for recovery is favorable.
A multidisciplinary approach involving dermatologists, obstetricians, and immunologists is essential for optimizing treatment outcomes while minimizing risks to the fetus.