- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2025. 15; 2. DOI 10.35630/2025/15/2.210
Aims: This review aims to compare the long-term clinical outcomes of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) in patients with left main coronary artery disease (LMCAD). It explores survival rates, major adverse cardiovascular and cerebrovascular events (MACCE), repeat revascularization, and the influence of patient-specific factors and optimal medical therapy (OMT) on treatment efficacy.
Methods: A structured literature review was conducted using PubMed, MEDLINE, Scopus, and the Cochrane Library to identify relevant randomized controlled trials, meta-analyses, and large-scale observational studies published from 2016 to 2025. A total of 37 studies meeting predefined inclusion criteria were reviewed, focusing on long-term outcomes (≥5 years).
Results: CABG offers superior long-term survival and durability compared to PCI, especially in patients with complex coronary anatomy, diabetes, or prior cerebrovascular disease. For example, the NOBLE trial reported a 5-year MACCE rate of 29% for PCI versus 19% for CABG. While short-term results appear similar, CABG significantly reduces long-term MACCE and repeat revascularization. PCI, however, is associated with fewer early strokes and shorter recovery. While most studies indicate CABG superiority in high-risk patients, some analyses suggest comparable outcomes in lower-risk individuals. OMT, particularly the use of dual antiplatelet therapy, high-intensity statins, and lifestyle modifications, has been shown to reduce event rates across both CABG and PCI groups.
Conclusions: CABG remains the preferred long-term strategy in complex LMCAD, though procedural choice should be individualized. Future studies should focus on refining patient selection criteria, exploring hybrid strategies, and assessing newer-generation DES in LMCAD treatment.
Left main coronary artery disease (LMCAD) is one of the most severe forms of coronary artery disease (CAD). It’s carrying a high risk of morbidity and mortality if left untreated. The left main coronary artery supplies a significant portion of the myocardium. Obstruction of this artery can lead to extensive ischemia and in the result life-threatening arrhythmias and myocardial infarction. Given the critical nature of this condition, timely and effective revascularization is essential to improving survival and quality of patients life. But which treatment procedure is better - coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI)? It remains a topic of ongoing debate.
Over the years, advancements in both surgical and interventional techniques have reshaped the treatment landscape for LMCAD. CABG has been the gold standard, for many years. It has been particularly for patients with complex coronary anatomy and high SYNTAX scores. The use of arterial grafts, such as the internal mammary artery, has been shown to provide long-term durability and reduce the need for repeat interventions. But with the introduction and refinement of drug-eluting stents (DES), PCI has emerged as a viable alternative. PCI is used in particular for patients with lower anatomical complexity or those at high surgical risk.
Despite numerous clinical trials comparing these two approaches, there is no universally accepted "one-size-fits-all" solution. Short-term outcomes appear similar between CABG and PCI. Long-term results often favor CABG in terms of survival, prevention of major adverse cardiovascular and cerebrovascular events (MACCE), and lower repeat revascularization rates. Meanwhile, PCI offers the advantage of a less invasive procedure, shorter recovery times, and lower initial stroke risk, what is making it an appealing option for many patients.
The choice between CABG and PCI is particularly complex when considering patient-specific factors such as diabetes, chronic kidney disease (CKD), previous cerebrovascular disease, left ventricular function, and frailty. Furthermore, the role of optimal medical therapy (OMT) in post-revascularization management has gained increasing attention. Statins, antiplatelet agents, and renin-angiotensin system inhibitors significantly influence long-term outcomes.
This review aims to compare the long-term survival and clinical outcomes of CABG versus PCI in patients with LMCAD. It is needed to analyze the risk of stroke, myocardial infarction (MI), and MACCE associated with each approach and to evaluate the impact of repeat revascularization and procedural durability. In this article we also want to assess how patient-specific factors influence treatment decisions, particularly in high-risk populations such as those with diabetes, CKD, and prior stroke and discuss the very important role of OMT in improving long-term prognosis.
By synthesizing the latest clinical trials, meta-analyses, and real-world registry data, this review aims to provide clinicians with a clear, evidence-based perspective on the most effective long-term treatment strategies for LMCAD. The choice of a procedure that fits best for patient isn’t always easy. This study should bring more confidence in decision making of which treatment procedure to choose – PCI or CABG.
This review was conducted to analyze and compare the long-term clinical outcomes of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) in patients with left main coronary artery disease (LMCAD). A systematic search was performed across four major databases—PubMed, MEDLINE, Scopus, and the Cochrane Library—to identify relevant studies published in English between 2016 and 2025.
Inclusion criteria:
The literature selection process was conducted independently by two reviewers to minimize bias. In case of disagreement, a consensus was reached through discussion. Data extraction focused on long-term clinical outcomes, and where applicable, results from meta-analyses were prioritized.
Although this is a review article, methodological quality and risk of bias were assessed qualitatively based on study design, sample size, duration of follow-up, and reporting transparency. Descriptive synthesis was performed. Where statistical comparisons between CABG and PCI were reported, effect estimates such as hazard ratios (HRs), odds ratios (ORs), and confidence intervals (CIs) were extracted and presented. However, no pooled meta-analysis was conducted as part of this review.
Since no new patient data were collected, Institutional Review Board (IRB) approval was not required. All sources used were openly available and appropriately cited to ensure academic integrity and reproducibility.
A total of 45 full-text articles were initially identified and assessed for eligibility. After removing duplicate studies and excluding those that did not meet the inclusion criteria, 37 studies were selected for final review. Among the 37 included studies, the research covered multiple key aspects of PCI vs. CABG in LMCA patients:
Moreover the studies were categorized into the following subsections to facilitate analysis:
Some studies were used in more than one category, because they presented data for more than one subsection.
Studies comparing the long-term outcomes of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) in left main coronary artery disease (LMCAD) evaluate survival rates over 5 and 10 years.
CABG and PCI showed similar survival rates within the first 5 years. There were also no significant differences in mortality. [2, 7, 22, 30, 36]. During 10 years observation CABG showed survival benefits. Especially among group of patients with more complex coronary anatomy [3, 4, 5, 9, 21, 29, 33]. In five randomized clinical trials (RCTs) there were no significant difference in overall mortality between PCI and CABG. But it is worth to mention that CABG significantly reduced the need for repeat revascularization [2, 5, 30]. The SYNTAXES study, which contain observations of the patients for 10 years, found lower all-cause mortality in the CABG in comparison to PCI. Particulalry in the group of patients with a history of cerebrovascular disease [6, 33, 36]. The NOBLE trial analysis indicates that 10-year survival was 80% for CABG and 48% for PCI. This conclusion confirms that CABG has a long-term advantage in the subject of survival [1, 22, 29]. In the MAIN-COMPARE registry are some findings that after 5 years, mortality increasing progressively in the PCI group. That occurs particularly among patients with left main bifurcation disease [14].
Both CABG and PCI carry significant risks of stroke, myocardial infarction (MI), and major adverse cardiovascular and cerebrovascular events (MACCE) in patients with left main coronary artery disease (LMCAD). However, these risks vary depending on patient characteristics, procedural complications, and long-term follow-up.
In a meta-analysis evaluating the impact of time on PCI versus CABG efficacy found that PCI initially showed lower rates of MACCE at 30 days compared to CABG. However this advantage lost over time. In the 3-year and 5-year periods PCI was associated with much more MACCE rates, though no direct increase in stroke or MI incidence was observed compared to CABG (25). At the 5-year follow-up, the MACCE rate was lower in the CABG group. There were fewer myocardial infarctions and repeat revascularizations [1, 2, 3, 5, 6, 7, 27, 30, 36]. At 10 years, the risk of MACCE was significantly higher in PCI. That suggest patients have worse long-term outcomes while undergoing PCI [21, 33]. The LE MANS study which is a 10-year follow-up showed similar mortality rates between PCI and CABG. On the other hand MACCE rate was higher in PCI patients [2, 5]. The SYNTAX trial analysis indicates that CABG patients reported fewer angina symptoms. Further more they required fewer additional interventions [1, 36].
A study from the EXCEL trial found that nonfatal periprocedural adverse events significantly affected 5-year mortality in both PCI and CABG patients. The occurrence of any major adverse event (MAE) within 30 days was a strong independent predictor of mortality. Notably, stroke and renal failure were much more associated with increased mortality only after CABG. Periprocedural stroke occurred in 0.6% of PCI patients versus 1.3% of CABG patients. At the 5- year follow-up, stroke was more common in CABG patients and has more mortality risk. MI was reported in 4.0% of PCI patients and 6.4% of CABG patients within the first 30 days. It shows slightly higher early procedural risk for CABG [15]. CABG was associated with significantly higher rates of major bleeding, arrhythmias, and prolonged intubation, which may contribute to increased mortality risk in a comparison to PCI [15]. In contrast, a 5-year analysis found that CABG reduced the risk of myocardial infarction compared to PCI. That showed that the CABG has more long-term durability and lower risk of ischemic events. [5, 7, 29, 30]
CABG particularly reduced the risk of myocardial infarction compared to PCI during 5-year observations [5, 7, 29, 30]. The LE MANS study (10-year follow-up) found similar MI rates between PCI and CABG, but CABG had a trend toward better MACCE-free survival [5, 21]. CABG was associated with a higher early stroke risk, but long-term stroke rates were similar between the two procedures [30, 32, 33, 35, 36].
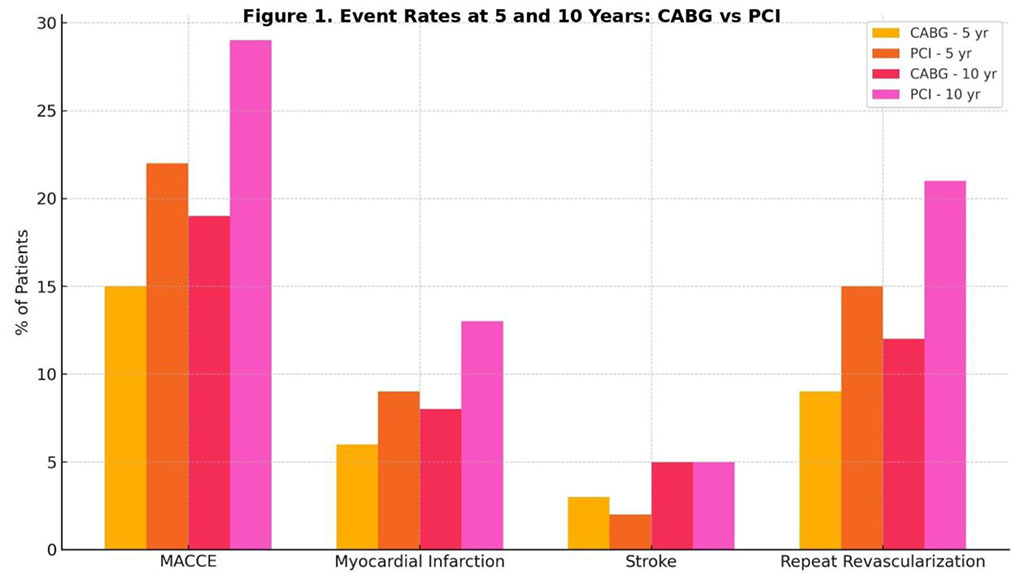
Figure 1. Comparative Incidence of MACCE, MI, Stroke, and Repeat Revascularization at 5 and 10 Years
Repeat revascularization remains a significant concern in patients undergoing percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) for left main coronary artery disease (LMCAD). Despite advancements in stent technology and surgical techniques, the durability of the initial revascularization differs between PCI and CABG, affecting long-term outcomes.
Studies show that PCI is associated with a significantly higher probability of repeat revascularization in comparison to CABG. In the EXCEL trial, the 3-year repeat revascularization rate was significantly higher in a group of patients treated by PCI (12.9% in PCI group vs. 7.6% in CABG group) [13]. During 5 years after treatment, the need for repeat revascularization was nearly twice as high in PCI compared to CABG (14.5% vs. 8.9%) [5, 6, 30]. At 10 years, PCI patients underwent almost twice as many repeat procedures compared to CABG [1, 2, 7, 33]. Most repeat revascularization procedures took place after 6 months post-intervention. That shows the early durability of both strategies are good, but after this period PCI becomes more negative. The primary causes of repeat revascularization were for PCI stent thrombosis, and it was responsible for 7.1% of repeat procedures. For CABG - graft occlusion was the cause of 62.7% of repeat interventions. It suggests difference failure mechanisms between the two ways of treatment [13].
The SYNTAXES study evaluates the impact of repeat revascularization within 5 years on 10- year mortality. It indicates that patients who underwent repeat revascularization had a higher 10- year mortality rate compared to those who did not (28.2% vs. 26.1%). The mortality difference was more demonstrate in patients initially treated with PCI (33.5% vs. 17.6%) than in those initially treated with CABG. However, in the overall cohort, repeat revascularization was not an independent predictor of 10-year all-cause mortality [34].
In the EXCEL trial, repeat revascularization was independently associated with an increased risk of 3-year mortality - all-cause mortality and cardiovascular mortality [13]. CABG provides greater long-term durability due to the use of arterial grafts, which are less prone to restenosis compared to stents used in PCI. Patients undergoing repeat revascularization after PCI had significantly worse survival rates in comparison to those undergoing repeat procedures after CABG [34].
The SYNTAXES study demonstrated that patients undergoing repeat revascularization after initial PCI had higher mortality rates than those undergoing repeat revascularization after CABG (33.5% vs. 17.6%) (34). Redo-CABG carries higher procedural risks than repeat PCI. This is making the choice of initial revascularization critical for long-term outcomes [1, 21, 22].
The SYNTAX score is a very important tool in managing for revascularization strategies in patients with left main coronary artery disease (LMCAD). It guides the selection of PCI and CABG.
The SYNTAX score II integrates anatomical and clinical factors. It has been validated as a predictor of long-term mortality after PCI or CABG in patients with multivessel and/or unprotected LMCAD. A study analyzing data from the BEST and PRECOMBAT randomized trials demonstrated that the SYNTAX score II had good calibration, however only moderate discrimination ability for long-term mortality prediction. The predictive value was higher for PCI than CABG. Patients who received treatment inappropriate to their SYNTAX score II recommendation had higher mortality in comparison to those treated according to the model’s prediction. These findings shows that the SYNTAX score shouldn’t be always considered into the heart team’s decision-making process to optimize selcetion between PCI or CABG [28].
The EXCEL trial showed how lesion site within the left main coronary artery (LMCA) affects revascularization outcomes. The study categorized patients based on lesion location to distal bifurcation disease and isolated ostial or shaft disease. The key findings were that at 3 years, the composite endpoint of death, myocardial infarction, or stroke did not vary remarkably between PCI and CABG for both lesion types. Repeat revascularization was significantly higher in PCI-treated patients with distal bifurcation disease (13.0% vs. 7.2%) in comparison to ostial/shaft disease. These findings point out that patients with high SYNTAX scores and distal bifurcation disease may benefit more from CABG. However PCI remains a workable option for patients with isolated ostial/shaft disease [10].
1.1.1. Impact of SYNTAX Score on Outcomes Based on Ejection Fraction
A sub-study from the EXCEL trial investigated how left ventricular ejection fraction (LVEF) influences revascularization outcomes in patients with LMCAD. The study divided patients into three groups: heart failure with reduced ejection fraction (HFrEF) (<40%), heart failure with mid-range ejection fraction (HFmrEF) (40–49%) and preserved ejection fraction (≥50%). The observation was that the patients with HFrEF had significantly worse outcomes within a 3-year period for both, PCI and CABG. Patients with HFmrEF and preserved LVEF had similar event rates between PCI and CABG too. The SYNTAX score was higher in patients with reduced LVEF and this suggests that patients with impaired ventricular function should be very carefully selected for PCI or CABG using their SYNTAX scores. It shows the importance of integrating LVEF status into decision-making along with the SYNTAX score [31].
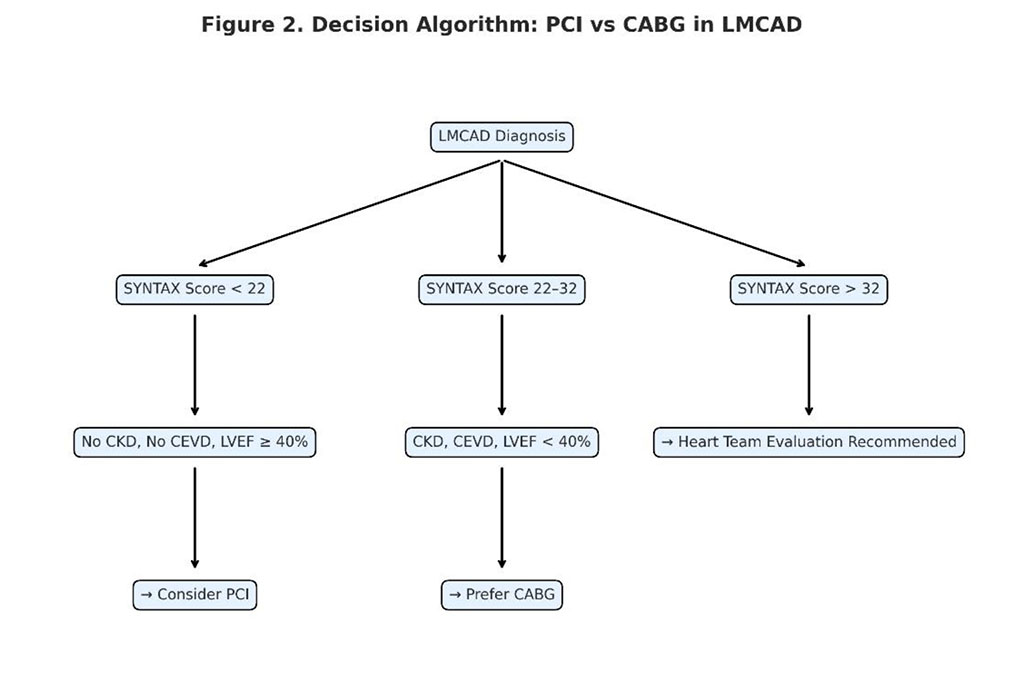
Figure 2. Decision algorithm for revascularization in LMCAD based on SYNTAX score and major clinical factors (CKD, CEVD, LVEF).
Patients with type 2 diabetes mellitus undergoing revascularization for LMCAD have been extensively studied, with varying outcomes between PCI and CABG. Meta-analyses and largescale trials indicate that CABG is superior for long-term outcomes in diabetic patients. The most significant was that the CABG had reduced major adverse cardiac and cerebrovascular events (MACCE) and lower repeat revascularization rates. But, CABG had a higher initial risk of stroke in comparison with PCI. A 10-year meta-analysis demonstrated that diabetic patients undergoing PCI had significantly higher rates of mortality compared to CABG. Despite this, CABG was associated with a nearly double higher risk of stroke (32, 35). The need for repeat revascularization was significantly higher with PCI than CABG. It highlights the long-term durability of surgical intervention (20, 32, 35). Subgroup Analysis in EXCEL Trial is the study that showed that at 3-year follow-up, diabetic and non-diabetic patients had similar rates of composite primary endpoints after PCI and CABG. On the other side all-cause mortality at 3 years was higher in PCI patients. These finding is indicating a potential long-term benefit of CABG (20).
Patients with CKD who are undergoing revascularization for LMCAD have higher procedural risks. Particularly regarding acute renal failure (ARF) and long-term mortality. CABG and PCI have shown similar survival outcomes, though CABG has a higher short-term risk of ARF. Patients with CKD had an increased rate of ARF, which was strongly associated with 3-year mortality. However, ARF was less frequent in PCI than CABG patients. The 3-year mortality rates were comparable between PCI and CABG in CKD patients [12]. A systematic review and meta-analysis further supported these findings, revealing that PCI-treated CKD patients had significantly higher MACCE rates, because of increased myocardial infarction and revascularization needs. Though PCI patients had higher mortality, the difference was not statistically significant [11]. Up to increased risks of renal dysfunction post-surgery, PCI may be preferable for certain CKD patients, despite its higher long-term need for repeat revascularization. On the other hand, CABG appears to provide better long-term durability, particularly in reducing the risk of MI and the need for subsequent procedures [11, 12].
Patients with a history of cerebrovascular disease (CEVD), including prior stroke or transient ischemic attack (TIA), present a particularly high-risk subgroup in LMCAD revascularization. Due to heightened risk of stroke-related complications, selecting the optimal revascularization strategy between CABG and PCI remains a key challenge. Patients with prior CEVD had a significant higher risk of stroke at 30 days and 3 years as well in comparison to those without CEVD [8]. CABG was associated with a higher perioperative stroke risk than PCI. However, long-term mortality rates were comparable between CABG and PCI [32]. A 10-year follow-up analysis indicated that patients with prior strokes had higher MACCE rates in PCI but lower stroke recurrence than those who underwent CABG [35]. The composite endpoint of death, stroke, or MI at 3 years was significantly higher in CEVD patients compared to non-CEVD patients. This increased risk was associated with higher incidence of stroke rather than MI [8]. In contrast, CABG was related with a lower long-term risk of repeat cerebrovascular events, despite its higher procedural stroke risk [32, 35]. A study from the EXCEL trial found no significant difference in stroke rates between PCI and CABG in CEVD patients. That is indicating that long-term stroke risk equalizes over time. On the other hand PCI was associated with a higher risk of MI in CEVD patients, while CABG was related with higher procedural stroke rates [8].
COPD is a known risk factor for cardiovascular mortality. The disease is the risk factor that is influencing the choice between PCI and CABG. Studies suggest that COPD patients undergoing CABG may have higher procedural mortality. By now, PCI may not offer a long-term survival advantage. COPD patients had significantly higher 10-year mortality rates compared to non-COPD patients. CABG was associated with slightly lower mortality than PCI in COPD patients. This difference however, was not statistically significant. Due to higher surgical risks, PCI may be the preferred option for COPD patients, but long-term outcomes require further investigation [37].
Women undergoing coronary revascularization often have higher baseline comorbidities and distinct clinical profiles compared to men, which may influence procedural outcomes. In the EXCEL trial, women undergoing PCI had higher rates of periprocedural myocardial infarction than men. On the other hand men had worse outcomes after CABG. There was no significant sex-based difference in the 3-year composite primary endpoint. The exception was a trend toward worse outcomes following PCI for a women group [26].
Optimal Medical Therapy (OMT) plays a crucial role in determining long-term outcomes for patients undergoing PCI or CABG for left main coronary artery disease (LMCAD).
The SYNTAX Extended Survival (SYNTAXES) study investigated the impact of OMT adherence on 10-year all-cause mortality among patients treated with PCI or CABG. The study revealed a significant survival benefit associated with adherence to OMT at 5 years. Patients who were on OMT (defined as the use of at least one antiplatelet drug, a statin, an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB), and a beta-blocker) at 5 years had significantly lower mortality at 10 years compared to those taking fewer than two of these medications. Patients taking three types of medications also experienced a similar mortality benefit to those on full OMT, suggesting that even partial adherence to guideline-recommended therapy can significantly improve outcomes [17].
A further breakdown of the data demonstrated that individual components of OMT had independent associations with survival. The use of antiplatelet therapy and statins at 5 years was associated with lower all-cause mortality at 10 years. These findings suggest that maintaining these medications post-revascularization is crucial for long-term survival. While the use of ACE inhibitors/ARBs and beta-blockers also contributed to mortality reduction. The association was less pronounced compared to antiplatelet agents and statins. However, beta-blockers leaded to a survival advantage, particularly in patients undergoing PCI (17).
The impact of OMT was also analyzed in the context of the mode of revascularization. Among CABG patients who were on antiplatelet therapy and statins at 5 years had significantly lower 10-year mortality than those who were not. This suggests that adherence to secondary prevention medications is particularly important in surgically treated patients. Although PCI patients also benefited from OMT. The impact was slightly lower compared to CABG patients. However, patients who did not adhere to OMT had significantly higher rates of repeat revascularization and myocardial infarction over the 10-year period. (17)
Over the past decade, the field of percutaneous coronary intervention (PCI) has undergone significant technological transformation. Among the most notable innovations are bioresorbable vascular scaffolds (BVS), designed to provide temporary vessel support and drug delivery, followed by complete biodegradation. Although early-generation BVS—such as Absorb—were associated with increased risk of late thrombosis and target lesion failure, newer platforms have demonstrated improved mechanical properties and safety profiles. These devices aim to restore natural vessel function and eliminate long-term foreign body presence, potentially lowering the risk of chronic inflammation and late stent thrombosis [11, 13, 20].
In parallel, third-generation drug-eluting stents (DES) incorporating bioresorbable or biocompatible polymer coatings have significantly improved outcomes in terms of in-stent restenosis and thrombosis. These DES platforms, evaluated in long-term comparative studies such as EXCEL, LE MANS, and SYNTAXES, have shown competitive safety and efficacy versus coronary artery bypass grafting (CABG) in selected patients with low to intermediate anatomical complexity [5, 6, 13].
In addition to stent design evolution, adjunctive diagnostic tools have played an increasingly central role in contemporary PCI strategy. Intravascular ultrasound (IVUS), optical coherence tomography (OCT), and fractional flow reserve (FFR) are routinely used to optimize lesion assessment, stent deployment, and procedural planning. Studies have demonstrated that IVUS-guided PCI is associated with reduced adverse events and improved long-term outcomes compared to angiography-guided procedures [10, 28].
Equally important are algorithmic approaches to individualized treatment strategy selection. The SYNTAX Score II, for instance, integrates clinical and anatomical variables—including age, renal function, LVEF, and anatomical lesion complexity—to provide personalized mortality predictions for PCI and CABG. Evidence from the EXCEL and PRECOMBAT trials supports the clinical utility of SYNTAX Score II in guiding heart team decisions, especially when applied to patients with unprotected left main coronary artery disease (LMCAD) [28, 31].
These technological and analytical advances have helped reframe the debate between CABG and PCI not as a binary choice but as a tailored, patient-specific decision, increasingly supported by quantitative tools and high-resolution imaging modalities.
This review includes a detailed analysis of how anatomical (e.g., SYNTAX score, lesion location in the left main coronary artery, distal bifurcation involvement) and clinical factors (e.g., diabetes, chronic kidney disease, prior stroke, reduced left ventricular ejection fraction, COPD, sex) affect revascularization choice and long-term outcomes. Evidence from studies such as EXCEL, SYNTAXES, PRECOMBAT, and LE MANS indicates that tailoring treatment to these variables significantly improves survival and reduces complications following PCI or CABG [1, 6, 10, 11, 12, 20, 26, 28, 31, 32, 35, 37]. A high SYNTAX score and distal bifurcation lesions favor CABG [10, 28], while patients with isolated ostial or shaft lesions may have comparable outcomes after PCI [10]. Diabetic and CKD patients derive greater long-term benefit from CABG, despite an increased perioperative stroke risk [11, 12, 20, 32, 35]. Patients with prior cerebrovascular disease (CEVD) are especially vulnerable to both stroke and MI regardless of the strategy, which calls for individualized risk-benefit assessment [8, 32, 35]. Left ventricular ejection fraction (LVEF) is another critical determinant—patients with HFrEF (<40%) show worse outcomes with either strategy, and higher SYNTAX scores are particularly unfavorable in this group [31]. Women and patients with COPD also require careful evaluation, although available data are more limited [26, 37].
The long-term outcomes of coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) in patients with left main coronary artery disease (LMCAD) remain a subject of ongoing debate. While both revascularization strategies have demonstrated efficacy in the short term, significant differences emerge over extended follow-up periods. This review highlights the key findings from multiple studies, emphasizing survival rates, major adverse cardiovascular and cerebrovascular events (MACCE), repeat revascularization, and the role of patient-specific factors in treatment selection.
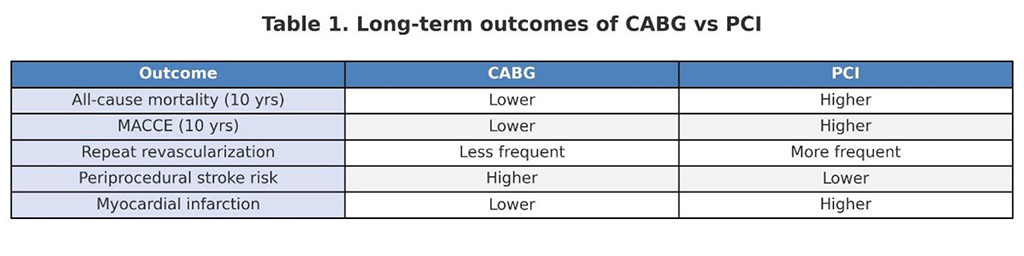
Table 1. Long term outcomes of CABG vs PCI
One of the most striking conclusions from the reviewed literature is that CABG and PCI exhibit comparable survival rates within the first five years post-procedure, with no significant differences in mortality. However, long-term survival at 10 years favors CABG, particularly among patients with complex coronary anatomy or high SYNTAX scores. These findings align with results from landmark trials such as SYNTAXES, NOBLE, and MAIN-COMPARE, which reported a progressive increase in mortality in PCI patients beyond the five-year mark.
Moreover, the risk of MACCE significantly increases over time in PCI-treated patients, largely due to a higher need for repeat revascularization. Although PCI initially demonstrates a lower incidence of MACCE, this advantage diminishes by the third year post-procedure. By year five, CABG provides greater protection against major cardiovascular events, including myocardial infarction (MI) and repeat interventions. The long-term durability of CABG, particularly in preventing MI and ensuring graft patency, appears to be a key factor in its superiority for long-term outcomes.
The need for repeat revascularization remains a major limitation of PCI, as evidenced by higher rates of subsequent interventions in PCI-treated patients across multiple studies. Despite advancements in stent technology, restenosis and stent thrombosis continue to contribute to the increased necessity for repeat procedures in PCI recipients. Conversely, CABG, through the use of arterial grafts (especially internal mammary artery grafts), offers superior long-term vessel patency and reduces the likelihood of additional interventions.
Interestingly, patients requiring repeat revascularization after PCI have significantly worse survival outcomes than those undergoing repeat procedures after CABG. This raises an important clinical consideration—while PCI offers a minimally invasive initial approach, it may not be the optimal long-term solution for patients with complex coronary disease. The findings reinforce the importance of individualized procedural selection, particularly for patients with diffuse disease and high anatomical complexity.
The risk of stroke and myocardial infarction (MI) represents another crucial factor in treatment selection. Studies indicate that CABG carries a higher early periprocedural stroke risk, primarily due to embolic events during cardiopulmonary bypass. However, over the long term, the incidence of stroke equalizes between CABG and PCI patients, suggesting that the early procedural risk should be weighed against CABG’s long-term survival benefits.
Conversely, PCI is associated with a slightly lower early stroke risk but a higher long-term risk of MI due to stent-related complications. The higher incidence of late ischemic events and recurrent angina in PCI patients underscores the need for stringent long-term follow-up and optimal medical therapy (OMT) to mitigate these risks.
The review also highlights the impact of patient-specific factors, such as diabetes, chronic kidney disease (CKD), prior stroke, and left ventricular ejection fraction (LVEF), in guiding revascularization decisions. An essential conclusion of this review is the central role of individualized patient stratification based on anatomical and clinical parameters. Evidence from multiple studies highlights that factors such as high SYNTAX score, distal bifurcation involvement, reduced left ventricular ejection fraction, diabetes, chronic kidney disease, and cerebrovascular disease substantially influence long-term outcomes and procedural risk. These variables underscore that no single revascularization strategy suits all patients. Therefore, the use of risk-prediction tools like SYNTAX Score II and collaborative Heart Team decision-making remain pivotal in optimizing therapeutic choices between CABG and PCI. Among these, diabetic patients have been consistently shown to derive greater long-term benefit from CABG due to their heightened risk of MACCE and restenosis following PCI. Similarly, CKD patients face higher procedural risks with CABG, but long-term data suggest better MACCE prevention compared to PCI. Patients with a history of cerebrovascular disease (CEVD) require careful procedural selection, as they face elevated stroke risk irrespective of the chosen revascularization strategy. Although CABG has a higher perioperative stroke incidence, PCI has been linked to increased MI rates in this population, further complicating treatment decisions. For women undergoing PCI, data suggest a higher incidence of periprocedural complications compared to men, though further research is needed to determine whether sex-specific treatment modifications may improve outcomes. Similarly, COPD patients often present increased surgical risks, making PCI an appealing alternative, though long-term outcomes still favor CABG.
An essential aspect of long-term patient management is adherence to optimal medical therapy (OMT). The SYNTAXES study demonstrated that patients adhering to OMT for five years had significantly lower 10-year mortality rates, regardless of their initial revascularization strategy. Among OMT components, antiplatelet agents and statins have been identified as the most crucial in improving long-term survival. Notably, CABG patients appear to derive greater survival benefits from OMT than PCI patients, further reinforcing the need for aggressive secondary prevention measures following surgical revascularization.
Modern PCI technologies—including bioresorbable scaffolds and next-generation DES—have substantially improved the efficacy and safety of percutaneous revascularization in selected LMCAD patients. Additionally, the integration of intravascular imaging and algorithmic risk stratification tools, such as SYNTAX Score II, supports a more nuanced and personalized treatment selection process. While CABG remains the gold standard in anatomically complex or high-risk patients, the evolution of PCI devices and techniques allows for an evidence-based, individualized approach to coronary revascularization.
The insights derived from this review emphasize the need for individualized, patient-centered decision-making in LMCAD revascularization. While PCI continues to evolve with advancements in stent technology and intravascular imaging, CABG remains the gold standard for patients with complex coronary anatomy, high SYNTAX scores, and diabetes.
However, rather than viewing CABG and PCI as competing interventions, a hybrid approach that combines the strengths of both strategies may offer a promising alternative in select cases. Future studies should explore personalized treatment algorithms, incorporating SYNTAX scores, functional imaging, and novel biomarkers to refine procedural selection further.
Moreover, the role of emerging adjunctive therapies, such as dual antiplatelet therapy (DAPT) optimization and anti-inflammatory agents, should be investigated to enhance long-term outcomes following both CABG and PCI.
In summary, the choice between CABG and PCI in LMCAD is multifactorial and highly dependent on patient-specific variables. While PCI offers a less invasive option with comparable short-term outcomes, CABG provides superior long-term survival, reduced MACCE rates, and greater durability. The importance of comprehensive risk assessment, multidisciplinary heart team discussions, and strict adherence to OMT cannot be overstated in optimizing revascularization strategies for this complex patient population.
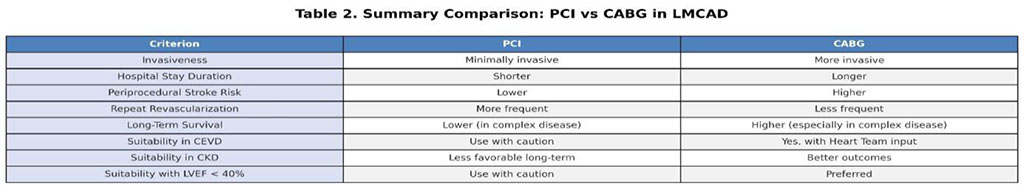
Table 2: Summary Comparison – PCI vs CABG in LMCAD