- Home
- About the Journal
- Peer Review
- Editorial Board
- For Authors
- Reviewer Recognition
- Archive
- Contact
- Impressum
- EWG e.V.
Cite as: Archiv EuroMedica. 2022. 12; 4: e1. DOI 10.35630/2199-885X/2022/12/4.17
The article presents the study of diagnostic methods and the use of autogenous connective tissue grafts in surgical methods of treating Miller class I gingival recession.
As the results, in the period from 2020-2021, 33 Miller class I gingival recession zones were treated. The height of gingival recessions before treatment averaged 3.5 ± 1.13 mm. Assessment of the level of attached keratinized gingiva up to the cement-enamel junction of the tooth showed a significant (p <0.001) increase after surgical treatment. The average percentage efficacy of recession coverage in the study group was - 84%. Pain, fibrinous plaque and soft tissue edema were insignificant. The use of free connective tissue autograft taken from the hard palate is an effective method of treating Miller class I gingival recession.
Keywords: gingival recession, surgical treatment, tunnel method, free connective tissue autograft
Currently, one of the major problems in the structure of dental diseases is periodontal disease. According to the World Health Organization (WHO), the level of periodontal disease in the working age population, namely in patients aged 35-45 years, reaches 98% [1].
One of the common forms of periodontal disease is gingival recession, which is a non-inflammatory displacement of the gingival margin in the apical direction from its physiological position with exposure of the root surface [2]. According to some domestic authors, the prevalence of gingival recession ranges from 9.7% at the age of 15 years and up to 99.3% in the adult population, while scientists note that the intensity and prevalence of gingival recession is increasing, which leads to the loss of periodontal attachment [3].
There are various treatments for gingival recession, including conservative treatment and surgical treatment. Medical methods of treatment exist and are applied, but the result is not persistent [4]. To increase the area of keratinized attached gingiva the "gold standard" is the use of a free connective tissue graft [5]. Thus, surgical treatment is the most predictable type of treatment, leading to a persistent increase in gingival volume, and is also an etiopathogenetic treatment, since not only the aesthetic defect and hypersensitivity of the tooth is eliminated, but also some of the etiological factors, significantly reducing the risk of root caries and tooth loss [6]. To date, success, characterized by the complete coverage of gingival recession, is predictable and possible in the early stages of the disease, namely, in class I-II Miller recessions, the treatment is not promising for class III and IV recessions [7].
Today early diagnosis of gingival recession is extremely important [8]. Thus, it is relevant to study diagnostic methods and the effectiveness of autogenous connective tissue grafts in surgical methods of treating Miller class I gingival recession.
Purpose of the study: To improve the efficiency of diagnosis and surgical treatment of class I gingival recession according to Miller using free connective tissue autograft from the hard palate.
33 patients (100%) were examined and treated with a diagnosis of Miller class I gingival recession at the Department of Therapeutic Dentistry, Bashkir State Medical University (Ufa, Republic of Bashkortostan, Russia) in the period from 2020-2021.
This study involved 14 men (42.4%) and 19 women (57.6%) aged 25 to 40 years. The maximum number of teeth with recessions in one patient corresponded to six teeth, the minimum number was 1 tooth.
The study involved patients who gave written informed consent to treatment, who considered themselves somatically healthy, who were not under medical supervision, and had no allergic history. The exclusion criteria were patients under 25 and over 40 years of age with decompensated somatic pathology, pregnancy and lactation, allergic history, and lack of informed consent to treatment in the framework of a scientific study.
A comprehensive examination of the patients was carried out according to the generally accepted standard technique, including: survey, external examination, examination of the oral cavity with filling in the periodontal card and determining the hygienic and periodontal indices. Surgical treatment was performed with OHI-S <1.6 and PBI <5%, which indicates the absence of clinically significant inflammation of the periodontal tissues.
During a clinical dental examination of the oral cavity, the height, width, prevalence of gingival recession, the width of the attached keratinized gingiva in the area of gingival recession, and the presence of anomalies of the frenum and mucous cords were assessed. A graduated periodontal probe with a graduation of 1 mm (HLW, Germany) was used to assess the metric indicators.
The height of the recession was determined by the distance from the cement-enamel border to the edge of the free gingiva along the central axis of the corresponding tooth (in mm). The width of the recession was defined as the distance between the medial and distal edges of the recession at the level of the cement-enamel junction of the corresponding tooth (in mm). The recession class was determined according to Miller's classification (P.D. Miller, 1985).

Figure 1. Installation of an intraoperative linear transducer L 8-18i - RS (8-18 MHz) wrapped in one layer of cling film in the hard palate (RF Patent No. 2722055 dated May 26, 2020).
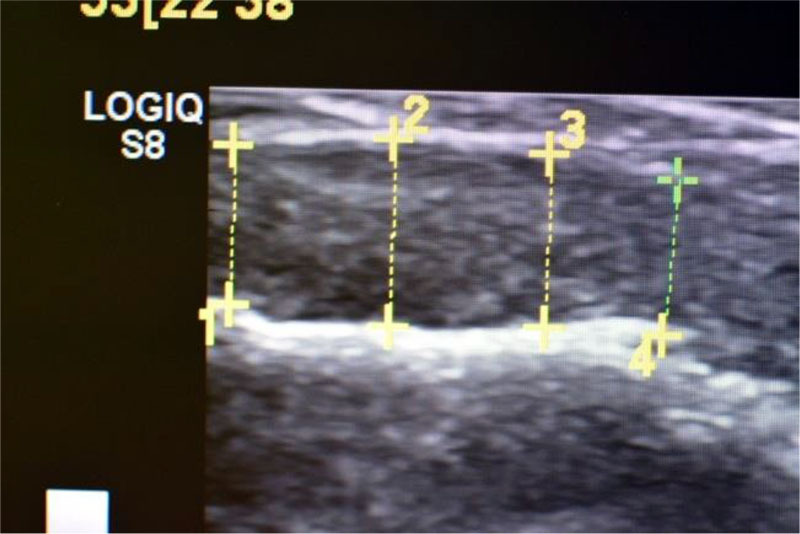
Figure 2. Registration of the obtained indicators of the thickness of the soft tissues of the oral cavity on the monitor screen during the ultrasound examination (RF Patent No. 2722055 dated May 26, 2020).
The biotype of the gingiva was determined using a non-invasive ultrasound examination using a specially developed method (RF Patent No. 2722055 dated May 26, 2020) (Fig. 1a, 1b). If the thickness of the gingiva is less than 1 mm, the biotype was considered thin; from 1.0 to 1.5 mm - average, when registering indicators over 1.5 mm, the biotype was considered thick [2].
Before the surgical intervention, all patients underwent a comprehensive professional oral hygiene (Scaling & Root Planning).
All patients (100%) underwent surgical treatment of gingival recession using a two-layer technique for eliminating multiple and single recessions using a modified tunnel method [9]. A free connective tissue autograft obtained from the hard palate was used as a graft.
The study group included patients who gave a written consent for the incision of their own autogenous tissue from the hard palate. Under infiltration anesthesia, using a microsurgical scalpel and a tunnel raspator, a mucous split flap (“tunnel”) was formed in the area of gingival recession according to the technique. The exposed roots of the teeth were treated mechanically and medically (lincomycin hydrochloride 30 mg / ml) for 2 minutes. A free connective tissue autograft was harvested from the hard palate according to the standard technique and installed in the receiving “tunnel bed” using 6.0 positioning sutures. The wound was closed with a 5.0 twist suture. Postoperative drug treatment was performed with 0.12% chlorhexidine solution.
All patients (100%) were given postoperative recommendations according to the standard protocol. Removal of sutures in both study groups was performed on the 14th day. Postoperative examination was performed on day 7, 14, after 1, 3 months. The result was assessed after 1 month. Long-term results were observed up to 3 months.
In the course of complex surgical treatment, a photo protocol was carried out in macro mode using: Canon 550D camera (Canon, Japan), Canon EF-S 60mm f / 2.8 Macro USM, Canon Macro Ring Lite MR-14 EX.
Evaluation of the effectiveness of the performed surgical intervention included the following criteria: patient satisfaction with the aesthetic result, absence of color and texture differences, thickness of keratinized gingiva after surgery,% elimination of gingival recession (100% corresponded to restoration of the free gingival margin to the cement-enamel border of the tooth), absence of pockets when probing, elimination of hypersensitivity.
The postoperative result of recession elimination was determined as the difference between the height of the existing recession before surgery and the height of the residual recession (on the 14th day after suture removal and 1 month after surgery) to the cement-enamel joint.
The degree of effectiveness of elimination of gingival recession was determined by the formula: 100% - (postoperative result of elimination of gingival recession * 100% / height of gingival recession before surgery). The result is expressed as a percentage (%).
In the postoperative period, during clinical examination, the following indicators were assessed in points:
Statistical processing of the studies was carried out in the GraphPadPrism v.6.0 for Windows program of the Microsoft Office system, using the Student's t-test. The data for which the probability of error p <0.05 was considered reliable. Differences were considered significant at p <0.05.
The main complaints in patients with Miller class I recession were hypersensitivity of the teeth due to bare roots, as well as aesthetic dissatisfaction. Bleeding was noted in 23% of cases. Supercontacts were found in 17 patients; in most patients (87%) with a generalized form of gingival recession, occlusion anomalies and crowding of teeth were found.
On clinical examination, hypersensitivity in the area of gingival recession was determined in 89% of cases, the presence of hyperemia in 21% of cases. 30% of the total number of patients were referred by dentists for periodontal treatment.
In terms of prevalence, localized gingival recession (within three teeth) was detected in 13 patients (39.4%), generalized in 20 patients (60.6%).
Ultrasound examination yielded the following results of the thickness of the attached keratinized gingiva out of the total number of patients (100%): thin biotype - the thickness of the gingiva in the recession area was 0.61 ± 0.19 mm; with an average gingival biotype, the thickness was 0.99 ± 0.1 mm; the thickness of the gingiva in patients with a thick biotype was 1.2 ± 0.17 mm. A thin biotype of the gingiva was detected in 18 patients (54.5%), an average biotype in 29 patients (33.4%), and thick in 4 patients (12, one%).
In the period from 2020-2021, 24 Miller grade I gingival recession zones were treated. The height of gingival recessions before treatment averaged 3.5 ± 0.09 mm, the width of the recessions corresponded to 4.00 ± 0.21 mm.
The dynamics of parametric measurements of gingival recession in patients before and after treatment are presented in Table 1.
Table 1. Dynamics of parametric measurements of gingival recession in patients before and after treatment.
| Before the treatment (baseline) | After the treatment | ||||
| for 14 days | in 1 month | ||||
| Gingival recession height (mm) | Thickness of keratinized gingiva (mm) | Gingival recession height (mm) | Thickness of keratinized gingiva (mm) | Gingival recession height (mm) | Thickness of keratinized gingiva (mm) |
| 4,0±0,2 | 0,79±0,09 | 0,8±0,07* | 2,8±0,03* | 1,1±0,04* | 1,9±0,08* |
* p <0.001 difference is reliable with baseline marked
The results obtained (Table 1) show that the height of the residual gingival recession and the resulting thickness of the keratinized gingiva on the 14th day after treatment are significantly higher than the initial level (p <0.001). The increase in the keratinized gingiva on the 14th day after treatment in the area of gingival recessions was 3.2 ± 0.13 mm, the increase in the thickness of the keratinized gingiva corresponds to 2.01 ± 0.03 mm.
When analyzing the clinical results obtained in the studied patients, the average% efficiency in eliminating class I gingival recessions according to Miller was 84%. The best clinical results were observed in the elimination of gingival recessions in the upper jaw. In 3 patients, the height of residual recession 1 month after treatment was 1.5 ± 0.03 mm in the area of the anterior teeth of the lower jaw, which is explained by the influence of the attachment of the frenum of the lower lip and mucous cords in this area.
This table shows that the method using free connective tissue autograft from the hard palate is an effective method of surgical treatment of Miller class I gingival recession. In addition, this method gives a stable, highly predictable result.
Evaluation of the elimination of recession and the height of the obtained attached keratinized gingiva to the cement-enamel junction of the tooth showed its significant (p <0.01) increase after surgical treatment in the studied patients.
Assessment of the severity of pain in the postoperative period showed similar ratios: the maximum values corresponded to 1 day after the surgical intervention - 1.78 ± 0.29 points, which significantly exceeded the severity of pain on 3-7 days of the postoperative period 0.2 ± 0.11 points. On days 7-14, pain sensitivity was completely absent.
Edema of soft tissues was insignificant, this indicator corresponded to 1.0 ± 0.3 points on days 2, 3, 7.
Fibrinous plaque and the consistency of the sutures were insignificantly expressed. The maximum indicators corresponded to 7 days - 1.85 ± 0.2 points. By 14-21 days, fibrinous plaque was absent.
Thus, in the studied patients after surgical treatment, fibrinous plaque and soft tissue edema were insignificant.
According to the data obtained, it can be concluded that the use of a free connective tissue autograft from the hard palate is an effective method of surgical treatment of Miller class I gingival recessions; moreover, this method allows obtaining a good and stable volume of attached keratinized gingiva.
Patient A., 32 years old. Diagnosis: By 06.01 Recession of the gingiva, Miller class I. Local recession in the region of the 43 tooth (Fig. 3). The biotype of the gingiva is medium (1.0 mm), the gingival papillae are normal. Orthodontic treatment is planned. Preoperative treatment of the oral cavity was performed with 0.12% chlorhexidine solution for 1 minute. Under infiltration anesthesia Sol. Ultracaini D-S 1.7 ml performed an intrasulcular incision using a microsurgical scalpel (MANI, Japan). The exposed surfaces of the roots of the teeth were carefully processed to the height of the loss of clinical attachment in 4 stages: ultrasonic treatment, instrumental machining using Gracie Mini-Five curettes (Hu-Friedy, USA), polishing and smoothing of the tooth root surfaces using periodontal burs RA (Komet, Russia), drug treatment with the application of lincomycin hydrochloride 30 mg / ml for 2 minutes. Tunnel raspatory (Hu-Friedy, USA) exfoliated the mucous split flap and prepared the tunnel bed. A free gingival autograft was taken from the hard palate (Fig. 4) and its de-epithelization (Fig. 5), adapted in size and introduced into the tunnel bed using guides positioning sutures PTFE 5.0 (Golnit, Russia) (Fig. 6). The wound was sutured using double twisted sutures PTFE 5.0 (Golnit, Russia) (Fig. 7). Postoperative drug treatment was performed with 0.12% chlorhexidine solution. Removal of stitches after 14 days. The result after 1 month is the complete elimination of gingival recession in the area of tooth 43, but unevenness of the keratinized gingiva is observed in the area of the base of the interdental papillae (Fig. 8).

Figure 3. Local recession of class I according to Miller in the region of the 43 tooth.
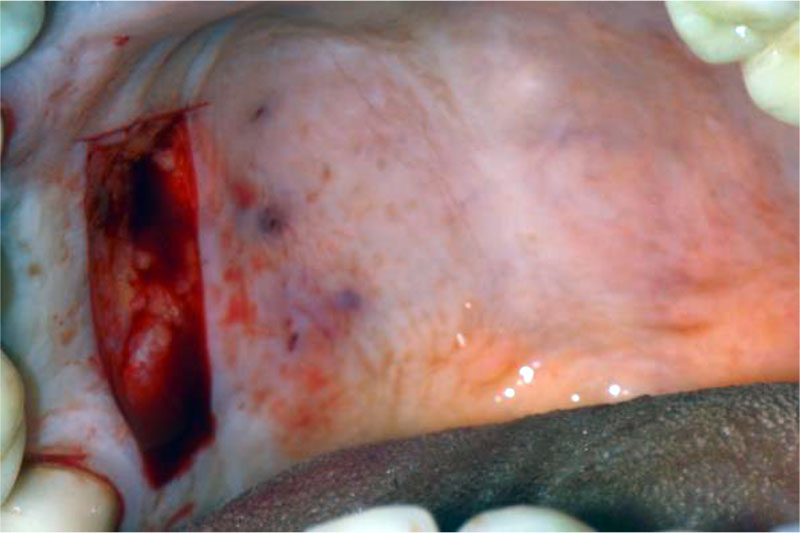
Figure 4. Elevating free gingival autograft from the hard palate.
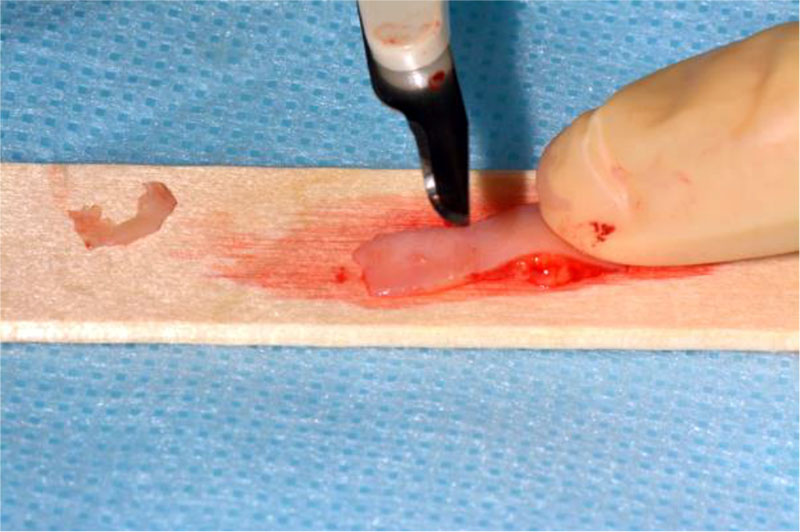
Figure 5. Obtaining a connective tissue subepithelial autograft by deepithelialization.

Figure 6. A free connective tissue autograft from the hard palate was introduced into the “tunnel bed” using PTFE 5.0 guide sutures (Golnit, Russia).

Figure 7. Suturing an operating wound using double twisted sutures PTFE 5.0 (Golnit, Russia).

Figure 8. Result in 1 month. Complete defect coverage in the area of 43 teeth. There is an additional volume of keratinized gingiva in the area of 43 teeth.